Introduction[]
“Partial mastectomy” and “lumpectomy” are the same thing—excisional biopsies that are taken out for masses, calcifications, or MRI enhancement, sometimes with an antecedent core biopsy. If a biopsy was done before, there may be a clip that was left in place to help find the area of interest later. The biopsy may be done either with or without wire localization.
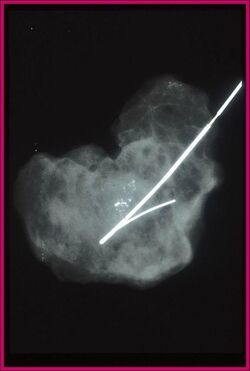
With Wire Localization[]
For wire localization biopsy (“needle loc”), the radiologist and breast surgeon arrange to place a wire through the lesion; the patient then goes to the operating room, with wire in place, to have the area around the wire resected. The specimen goes to radiology to be X-rayed before coming up to the pathology lab.
Note that while the wire helps the surgeon find the area to excise, it has no significance to the pathologist once the specimen is out, and can be removed. (Exception: if you need to match up the actual specimen with the specimen radiograph, in order to correlate some calcifications or a mass, the wire can help you with orientation.) Since the wire has a J-hook on the end, you may need to feed it forward through the specimen to remove it. You have no special duty to keep track of the part of the specimen that contained the wire.
Without Wire Localization[]
If the abnormality is clinically appreciable, palpable or otherwise large, wire localization is not needed and the surgeon just finds the area to excise by palpation. These specimens have no wire and are not radiographed.
Fresh Handling[]
Unoriented specimen[]
- Remove wire if present.
- Ink specimen entirely black.
- Fix in formalin and document time of fixation.
Oriented specimen[]
- Remove wire if present.
- Use the surgeon’s sutures to orient the specimen. Sometimes the specimens are far from cubical and the orientation therefore is hard to interpret. Do your best and ask for assistance if necessary.
- Measure specimen.
- Note: Since the tissue is soft, the dimensions of the specimen will depend on how it is lying on the table. Lay the specimen down as if it were still in the supine patient prior to measurement.
- Ink specimen in six colors.
- Superior blue (“blue sky”)
- Inferior green (“green grass”)
- Lateral yellow (both contain “L” twice)
- Medial violet (both contain “L” once)
- Anterior/superficial red
- Posterior/deep black
- Pat dry and treat with acetic acid. With so many colors, ink will run easily.
- Fix in formalin and document time of fixation.
Grossing In[]
Small specimen (<20 blocks): Submit in toto[]
- Breadloaf specimen to look for a lesion or clip.
- Note that calcs and MRI enhancement are not grossly visible.
- Describe background breast tissue (e.g., primarily fibrous, primarily adipose, 75% adipose).
- Describe lesion size (three dimensions), color, texture/consistency, and distance to two closest margins.
- Submit specimen in toto, with perpendicular submission of tips.
Huge specimen (usually >30 blocks): Submit selectively[]
- Breadloaf specimen to look for a lesion or clip.
- Note that calcs and MRI enhancement are not grossly visible.
- Describe background breast tissue (e.g., primarily fibrous, primarily adipose, 75% adipose).
- Describe lesion size (three dimensions), color, texture/consistency, and distance to two closest margins.
- Select areas to submit:
- If a definite lesion was found:
- 3-4 blocks of lesion.
- Relation between lesion and two closest margins (take section perpendicular to margin).
- One block perpendicular to each of the additional margins.
- If no definite lesion was found:
- Entirety of most suspicious area.
- Relation between suspicious area and two closest margins.
- One block perpendicular to each margin.
- If a clip was found:
- 3-4 blocks surrounding the clip.
- Relation between suspicious area and two closest margins.
- One block perpendicular to each margin.
- If a definite lesion was found:
- Consult attending if unsure.
Submit the case in a bucket designated for “breast”, “fat”, or “16 hour” processing (all of these mean the same thing).
Sample Dictation[]
The specimen consists of an oriented/unoriented “Partial Mastectomy/ Lumpectomy” specimen, measuring ___ x ___ x ___ cm, received with/without a localization wire. The requisition is labeled with the radiologist’s interpretation stating “____________“.
For unoriented specimens:
The specimen is received unoriented, with no specific suture designations and the external surface of the specimen is inked entirely black.
OR
For oriented specimens:
The specimen is received oriented, with a short suture indicating the (superior) margin and a long suture indicating the (lateral) margin of the specimen. The specimen is inked as follows: Superior : Blue; Inferior: Green; Anterior: Red; Posterior: Black; Medial: Violet; and Lateral: Yellow.
The specimen is serially sectioned to reveal
No grossly apparent lesions. A clip is/is not identified.
OR
An ill-defined, firm, fibrotic area, probably representing the prior biopsy site, is identified, measuring ___ x ___ x ___ cm, situated ___ cm from the lesion/mass and ___ cm from the closest ___ margin (margins)/ OR situated ___ cm from the superior, ___ cm from the inferior, ___ cm from the anterior, ___ cm from the posterior, ___ cm from the medial and ___ cm from the lateral margins./ OR abutting the ___ margin. A clip is/ is not identified in this prior biopsy site.
OR
A solitary/___, ovoid/round/irregular (spiculated), solid/cystic, well/poorly circumscribed, nodular mass, measuring ___ x ___ x ___ cm, ___- in color, firm/soft/hard/schirrous in consistency, well/poorly encapsulated, with a homogenous/heterogeneous cut surface, with/without areas of hemorrhage and necrosis, situated ___ cm from the closest ___ margin (margins)/ OR situated ___ cm from the superior, ___ cm from the inferior, ___ cm from the anterior, ___ cm from the posterior, ___ cm from the medial and ___ cm from the lateral margins./ OR abutting the ___ margin. (An ill-defined, firm, fibrotic area, probably representing the prior biopsy site, is identified, measuring ___ x ___ x ___ cm, situated ___ cm from the lesion/mass and ___ cm from the closest ___ margin (margins)/ OR situated ___ cm from the superior, ___ cm from the inferior, ___ cm from the anterior, ___ cm from the posterior, ___ cm from the medial and ___ cm from the lateral margins./ OR abutting the ___ margin. A clip is/ is not identified in this prior biopsy site).
Review and Signout[]
If there is invasive carcinoma, remember to add in the breast template in the "microscopic description" part of the report. You need to document all of the margins, and measure the DCIS and invasive ductal carcinoma from each margin which is less than 1.0 cm. If it is over 1.0 cm, then the margin is free of involvement. Also, you need to find what they did the biopsy for (microcalcs, mass), and make sure you see the corresponding finding on the slide. Sometimes this is the first-time diagnosis. Other times it's an excision of a tumor which was diagnosed with a core needle biopsy.
1. Right breast, ___ o’clock, needle localization partial mastectomy:
2. Right breast, ___ o’clock, partial mastectomy:
- Benign breast tissue with microcalicfications, see note.
- NOTE: The microcalcifications correlate with the radiologic findings on the specimen mammogram.
- Benign breast tissue with proliferative fibrocystic changes and microcalcifications, see note.
- NOTE: The microcalicficiations correlate with the radiologic findings on the specimen mammogram.
- Benign breast tissue with sclerosing adenosis.
- Fibroadenoma, xx cm.
- Ductal carcinoma in situ, (solid and/or cribiform) pattern(s), with (comedo-type necrosis and/or associated microcalcifications), (resection margins free of involvement) or (___ cm from the superior/inferior/etc. resection margin).
- A. Invasive ductal carcinoma, ___ cm, (well, moderately, poorly) differentiated, resection margins free of involvement) or (___cm from the superior/inferior/etc. resection margin), smd(F9).
- B. Associated ductal carcinoma in situ, solid and/or cribiform pattern(s) with comedo-type necrosis), (resection margins free of involvement) or (___ cm from the superior/inferior/etc. resection margin).
Return to Breast Grossing